1 s2.0 S1521690X0400020X Main PDF
Uploaded by
Veronika Nika1 s2.0 S1521690X0400020X Main PDF
Uploaded by
Veronika NikaBest Practice & Research Clinical Endocrinology & Metabolism
Vol. 18, No. 2, pp. 249–265, 2004
doi:10.1016/[Link].2004.03.010
available online at [Link]
Physiological and pathological aspects
of the effect of human chorionic
gonadotropin on the thyroid
Jerome M. Hershman* MD
Endocrinology-111D, VA Greater Los Angeles Healthcare Center, 11301 Wilshire Blvd, Los Angeles, CA 90073, USA
Human chorionic gonadotropin (hCG) is a glycoprotein hormone that has structural similarity to
TSH. At the time of the peak hCG levels in normal pregnancy, serum TSH levels fall and bear a
mirror image to the hCG peak. This reduction in TSH suggests that hCG causes an increased
secretion of T4 and T3.
Women with hyperemisis gravidarum often have high hCG levels that cause transient
hyperthyroidsm. In the vast majority of such patients, there will be spontaneous remission of the
increased thyroid function when the vomiting stops in several weeks. When there are clinical
features of hyperthyroidism, it is be reasonable to treat with antithyroid drugs or a beta-
adrenergic blocker, but treatment is rarely required beyond 22 weeks of gestation.
Hyperthyroidism or increased thyroid function has been reported in many patients with
trophoblastic tumors, either hydatiditform mole or choriocarcinoma. The diagnosis of
hydatidiform mole is made by ultrasonography that shows a ‘snowstorm’ appearance without
a fetus. Hydatidiform moles secrete large amounts of hCG proportional to the mass of the tumor.
The development of hyperthyroidism requires hCG levels of . 200 U/ml that are sustained for
several weeks. Removal of the mole cures the hyperthyroidism. There have been many case
reports of hyperthyroidism in women with choriocarcinoma and high hCG levels. The principal
therapy is chemotherapy, usually given at a specialized center. With effective chemotherapy, long-
term survival exceeds 95%.
A unique family with recurrent gestational hyperthyroidism associated with hyperemesis
gravidarum was found to have a mutation in the extracellular domain of the TSH receptor that
made it responsive to normal levels of hCG.
Key words: human chorionic gonadotropin; thyrotropin; pregnancy; hyperemesis gravidarum;
hydatidiform mole; choriocarcinoma; mutant thyroid-stimulating hormone receptor.
* Tel.: þ 310-268-3852; Fax: þ 310-268-4879.
E-mail address: jhershmn@[Link] (J.M. Hershman).
1521-690X/$ - see front matter Published by Elsevier Ltd.
250 J. M. Hershman
HCG BIOCHEMISTRY AND PHYSIOLOGY
Biochemistry
Human chorionic gonadotropin (HCG) is a member of the glycoprotein hormone
family that is composed of a common a-subunit and a hormone-specific b-subunit, non-
covalently associated.1 The a-subunit of HCG, that is common to the pituitary
hormones, thyroid-stimulating hormone (TSH), follicle-stimulating hormone (FSH) and
luteininzing hormone (LH), consists of a polypeptide chain of 92 amino acid residues
containing two N-linked oligosaccharide side-chains. The hCG b-subunit consists of
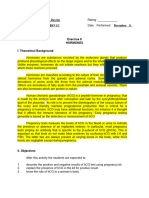
145 residues with two N-linked and four O-linked oligosaccharides. Figure 1 shows the
structure of the HCG subunits. The TSH b-subunit is composed of 112 residues and
one N-linked oligosaccaride. The b-subunits of both possess 12 half-cysteine residues
at highly conserved positions. Three disulphide bonds form a cystine knot structure,
identical in both hormones and essential for binding to the receptor.2 HCG and LH bind
to the same receptor.
A single gene on chromosome 6 encodes the a-subunit.3 The genes that encode the
b-subunits are in a cluster on chromosome 19. There are eight genes for the b-subunit
of HCG/LH. One gene codes for LH, and seven genes code for HCG, but only three are
actively transcribed. Only primates and horses have genes for b-HCG. A single base
deletion in the b-LH gene caused a read-through mutation of a stop signal in the b-LH
gene, resulting in the extended carboxyteminal 33 amino acid sequence of b-HCG.
HCG, molecular weight 36 700, contains 30% carbohydrate, the highest
carbohydrate content of any human hormone. In contrast with the approximate
1 hour plasma half-life of LH, that of HCG is about 24 hour because of its high sialic acid
content that prevents uptake and degradation by the liver. The complete hCG molecule
is synthesized primarily in the syncytiotrophoblast. Small amounts of the a and b
subunits are also secreted.
Pattern of secretion
Secretion of HCG begins very early in pregnancy and peaks at 9– 11 weeks of
pregnancy (Figure 2). Peak levels are in the range 30 –100 U/l and last for only a few
days, then gradually decline to a nadir of 5 –10 U/l at about 20 weeks, where they
remain throughout the latter half of pregnancy. The peak levels bear a relation to the
mass of the placenta. Peak levels are higher and more prolonged when there are
multiple fetuses.
Glycoprotein hormone receptors
The glycoprotein hormone receptors are members of the large superfamily of G-protein-
coupled seven-transmembrane receptors. They share a high degree of homology (, 70%)
in their transmembrane domains.4 The main differences are found in the large amino-
terminal extracellular domain involved in binding of the hormone. In the extracellular
domain, the LH/CG receptor has 45% homology with the TSH receptor.4 – 6
Function of HCG
The best known biological function of hCG is the maintenance of the function of the
corpus luteum, resulting in continued progesterone production. However, progesterone
Effect of human chorionic gonadotropin on the thyroid 251
α-subunit
20
Pro Glx Ser Phe Phe Pro
Gly Asx
Ala
Glx
Pro
1
H2N Ala Pro Glx Glx
Pro
Asx 7
Val 10 Leu
Glx
Asx Cys Cys Thr
Ile
28
Leu 40
Gln Cys Met Gly Cys Cys Phe Ser Arg Ala Tyr Pro Thr Pro
31 32 Leu
Asn Tyr Ser Lys Ala 59 Arg
Arg Val Cys
Val Cys
Thr Ser
60
Thr Ser
70 Val Glx Lys
Cys Tyr
Met Ser
Thr 87 Tyr Lys
Thr
Gly Ser Hls Arg
90 Lys Val
Gly 81 Cys Thr
Ser COOH
Val Asn Ser
Pha 82 Met
Thr Lys
Lys Cys CHO Gln
70 CHO Leu Lys
Val Ala Hls
Val Thr 50 Val
Hls
Met Glx Asn 80 Lys
Gly
Gly Pro Leu Val Thr
hCG β-subunit Ala
Leu 50 Gly
Phe
Pro Gln
Lys Gln
Leu
Val Val
57 Val
Arg Tyr Asn Cys
Glx Asp
Val
Val
Pro Thr
Arg Cys Arg
Thr Met
Phe Tyr 38
Asn Pro Val Glu
Val
Ser Val Gly
Gly Ile Ser
80 Tyr
Arg Arg Ala Ala
Val Gln
Leu Ala
Pro Pro Cys 34 93 Arg
Leu Arg eu
Gly Ser Ile Cys Ser
Cys
CHO Thr
26 Leu Thr
Pro Thr Cys 90
Val Cys Ile Thr Val Asn
88 Gln Ala
30 Cys
23 Thr
Gly Pro AspAsp CysThr Asp
Arg Leu Pro
Phe 110 Hls Asp Arg CysArg Lys Pro Gly Gly Cys
Glu Pro ProArg
Lys Ile 9 100
Leu
Glu Asn Pro
A Val Ala Ala Gln
Asp Leu Thr Lys
Val Ser CHO Ser
Ser H2N
Gly 120 Ser
CHO Ser
Arg Lys
Ala CHO CHO
72 Pro CHO 130 140
Pro Pro Gln COOH
ProSer Leu Pro Ser Pro Ser Arg Leu Pro Gly Pro Ser Asp Thr Pro Ile Leu Pro
Cys 145
Pro Val Cys 90
Cys Ile Thr Val Asn
Cys Gln Ala
30 88 Cys
23 Thr
Gly Pro Asp Asp Cys Thr Asp
Arg Leu Lys Pro Gly Gly Cys
Pro Hls Asp
Phe 110 Arg Cys Arg
Glu Pro Arg
Pro 100
Lys Ile 9 Leu
Glu Asn Pro
Gln Val Ala Gln
Asp Ala Leu Thr Lys
Ser CHO Ser
Ser H2N
1
120 Ser
CHO Ser
Lys
Ala CHO CHO
Pro CHO 140
130 COOH
Pro Gln
Ile Leu Pro
Pro Arg Leu Pro Gly Pro Ser Asp Thr Pro
Ser Leu Pro Ser Pro Ser 145
Figure 1. Schematic representations of the alpha and beta subunits of hCG (from Ren SC, Braunstein GD,
Sem. Reprod. Biol. 1992; 10:95 –105, reprinted by permission).
252 J. M. Hershman
1.5 50
40
)
)
1.0
hCG (I.U./Lx1000) (
30
TSH (mU/L) (
20
0.5
10
0
0 10 20 30 40
WEEKS OF GESTATION
Figure 2. Serum hCG and TSH as a function of gestational age. (with permission9). Q 1990 The Endocrine
Society.
synthesis by the corpus luteum begins to decline at about 6 weeks, several weeks before
peak hCG secretion. Until the seventh week of pregnancy, the survival of the pregnancy
depends on the steroids from the corpus luteum.
A second function of HCG is stimulation of fetal testicular secretion of
tesotosterone that attains a maximum at approximately the same time in gestation
when the maximal levels of hCG are attained. Thus, at a critical time in sexual
differentiation of the male fetus, hCG, entering fetal plasma from the syncytiotropho-
blast, stimulates the replication of fetal testicular Leydig cells and testosterone synthesis
to promote male sexual differentiation.
Thyrotropic action in normal pregnancy
At the time of the peak hCG levels in normal pregnancy, serum TSH levels fall and bear
a mirror image to the hCG peak7 – 9 (Figure 2). This reduction in TSH can now be
measured with precision with current sensitive TSH assays. The increase of HCG most
likely causes an increased secretion of T4 and T38,9, but this is difficult to establish with
certainty because the increased thyroxine-binding globulin (TBG) level of pregnancy
may confound the measurement of small changes in free thyroid hormone levels, and
data in the literature are contradictory. Several reports show that free T3 or T4 levels
are significantly elevated at the time when hCG levels are maximal.8 – 11 It is likely that
the HCG-induced thyroid secretion increases free T4 and free T3 levels, albeit
within the normal range. Thyroid-stimulating activity in sera of normal pregnant women
shows a significant correlation with serum hCG levels.12,13 In bioassays, hCG is only
about 1/104 as potent as hTSH during normal pregnancy.14 It is likely that the
thyrotropic activity of hCG during its peak secretion overrides the normal operation of
the hypothalamic-pituitary-thyroid feedback system.8,15
Effect of human chorionic gonadotropin on the thyroid 253
In a systematic survey of pregnant women in Brussels during the first trimester, 20%
had a suppressed serum TSH level and increased serum thyroxine concentration, and in
1% this was associated with clinical features of hyperthyroidism.16 In Asian women in
Singapore at 8 – 14 weeks of pregnancy, 33% had suppressed TSH and 11% had
suppressed TSH and elevated free T4 levels.17
Assays of thyrotropic action of HCG
HCG has thyroid-stimulating activity in bioassays in mice, rats, chicks and men.18 – 20
Administration of single doses of large amounts of commercial HCG to men cause the
release of thyroidal radiodidine, even though the peak HCG levels attained were only
25 –42 U/ml.21 HCG stimulates iodide uptake, adenylate cyclase, and DNA synthesis in
cultured rat thyroid cells.22 HCG stimulates iodide uptake by increasing the mRNA and
protein level of the sodium/iodide symporter.23 In Chinese hamster ovary (CHO) cells
transfected with the human TSH receptor, hCG increased adenylate cyclase and DNA
synthesis.24,25 These studies demonstrated unequivally that HCG activates the TSH
receptor and is a weak thyrotropin. LH and hCG lacking the C-terminal peptide of the
beta subunit were almost ten-fold more active in this system.25 In clinical situations such
as primary hypogonadism, the elevated levels of LH are several orders of magnitude
below those required to activate the TSH receptor.
Metabolism of HCG
The hCG immunoreactivity in serum is a mixture of hCG-related molecules, including
intact hCG, nicked hCG (missing the peptide linkage at b44 –45 or b47– 48),
carbohydrate variants of hCG, hCG missing b-C-terminal tail, hCG free a-subunit and
free b-subunit.26 Nicks of the hCG molecule frequently occur in a hydrophobic loop in
the hCG b-subunit, which is held in place by a disulfide link between Cys38 and Cys57
(Figure 1). Nicking of the hCG molecule may result from the deactivation and
degradation pathway of hCG in serum and urine.27 The nicking of the peptide bonds
reduces the binding of hCG to its receptor and causes a loss of 80% of its steriodogenic
activity.28 Nicked hCG preparations, obtained from patients with trophoblastic disease
and by enzymatic digestion of intact hCG, had approximately 1.5 –2-fold the potency of
intact hCG for stimulation of recombinant human TSH receptor.29 Therefore, the
thyrotropic activity of hCG is also influenced by the metabolism of the hCG molecule.
Role of carbohydrate in thyrotropic action of hCG
The biologic activity of glycoprotein hormones is influenced by the number and
structure of the oligosaccharide side chains. Extensive variations are possible in the
branched oligosaccharide structures, contributing to considerable heterogeneity of
glycoprotein hormones.30 Deglycosylation and/or desialylation of hCG enhances its
thyrotropic potency in rat (FRTL-5) thyroid cells.31,32 Basic hCG isoforms with lower
sialic acid content extracted from hydatidiform moles were more potent in activation of
adenylate cyclase, and showed a high ratio of bioactivity/immunoactivity (B/I) in CHO
cells tranfected with human TSH receptors.33 This is consistent with the finding that
the b-C-terminal tail-truncated hCG with higher thyrotropic potency is substantially
deglycosylated and desialylated in the b-subunit in comparison with intact hCG because
all four O-linked glycosylation sites occur within the missing C-terminal extension.25
Although removal of sialic acid from hCG enhances its TSH receptor binding, it also
reduces its plasma half-life because sialic acid blocks the high affinity for and rapid
254 J. M. Hershman
uptake of hCG by hepatic receptors for asialoglycoproteins.34 Therefore, it is likely that
the thyrotropic activity of hCG is regulated by two factors: the amount of desialylated
hCG produced from trophoblast cells and its plasma half-life.25 The precise nature of
the thyrotropic molecular variant of hCG is controversial. HCG that is less sialylated
activates the TSH receptor to a greater extent14, as has been reported in gestational
thyrotoxicosis.14 However, lack of sialic acid reduces its half-life. More acidic variants of
hCG have a longer half-life and, therefore, a more prolonged action.35,36
HYPEREMESIS GRAVIDARUM
Definition and prevalence
Hyperemesis gravidarum occurs in about 1.5% of pregnancies and is probably more
prevalent in Asian women than in Caucasians.37 The incidence is 4.5% in Kuwait.38 It is
characterized by prolonged and severe nausea and vomiting in early pregnancy that
leads to a loss of 5% body weight, dehydration and ketosis.39 It frequently results in
hyponatremia, hypokalemia, hypochloremic alkalosis, and abnormalities of liver
function. Other causes of vomiting must be excluded. There is a correlation between
the degree of vomiting and the serum hCG level (Figure 3).39 Management includes
hospitalization, intravenous fluid and electrolyte replacement, thiamine supplemen-
tation, conventional antiemetics, and psychological support.
Increased thyroid function
There are many reports of series of hyperemesis patients whose thyroid function has
been studied. A study in Belgium reported that free thyroxine index was increased in
25 of 33 consecutive hyperemesis patients, of whom six were treated with
methimazole until euthyroid.40 However, free thyroxine index normalized in all
patients, regardless of therapy. A study of 25 patients with hyperemesis in England
found that ten had increased free thyroxine levels.41 Those with increased free
thyroxine had suppressed TSH responses to thyrotropin-releasing hormone. The free
thyroxine levels normalized when the vomiting stopped and remained normal
postpartum. In contrast, a 39 year-old woman presented with severe hyperemesis at 8
weeks pregnancy and very high serum hCG level.42 Although she was treated with
methimazole suppositories until euthyroid at 18 weeks, her vomiting persisted until
delivery, suggesting that the vomiting was not caused by the increased thyroid function.
A study of 71 patients with hyperemesis in Hong Kong revealed that one-third had high
free T4 and one-fifth had high free T3 levels.43 In those with elevated free thyroid
hormone levels, serum hCG was higher. A study in Israel of 41 consecutive admissions
with hyperemesis showed that free thyroxine was increased in 11 patients.44 Four
were treated with propylthiouracil because of tachycardia, two of whom had goiter.
Thyroxine levels returned to normal in the untreated patients when the hyperemesis
abated. A study in Turkey of 24 patients with hyperemesis reported that their free T3,
free T4 and hCG levels were significantly higher than those of controls.45 Twin
pregnancies are more often associated with sustained elevation of hCG and
hyperemesis gravidarum.37,46
A prospective study of 57 consecutive patients with hyperemesis in Los Angeles
compared them with 57 women of similar gestational age.39 In the hyperemesis
patients, TSH was suppressed in 60%, free T4 was increased in 46%, while free T3 index
Effect of human chorionic gonadotropin on the thyroid 255
3.0
NO VOMITING (N-30)
VOMITING (N-27)
2.5
HYPEREMESIS (N-38)
SEVERE HYPEREMESIS (N=19)
2.0
TSH (mU/L)
1.5
1.0
0.5
0.0
40
30
free T4 (nmol/L)
NS
20
10
150
NS
125
100
bCG (IU/mol)
75
50
25
Figure 3. Relation between the severity of vomiting and serum concentratons of TSH, free T4, and hCG
(mean ^ SE). Hormone concentrations differed significantly between each group of patients except as
indicated by NS. (with permission39). Q 1992 The Endocrine Society.
256 J. M. Hershman
was increased in only 12%. The explanation for the relatively lower T3 compared with
T4 may be that caloric deprivation impaired conversion of T4 to T3. Serum HCG levels
were three-fold higher in the hyperemesis patients than in the controls (Figure 3). No
patient in this study had goiter or clinical features of hyperthyroidism. For the entire
group, the degree of biochemical hyperthyoidism and the hCG concentration
correlated with the severity of vomiting (Figure 3). There was an inverse correlation
between the serum HCG and the serum TSH levels and a direct correlation of HCG
with free T4 levels (Figure 4). Thyrotropic activity in the serum, estimated by bioassay,
250
200
Hyperemesis
Control
bCG (IU/ml)
150
100
50
0
0.0 1.0 2.0 3.0 4.0 5.0
TSH (mU/L)
250
200
150
hCG (IU/ml)
100
50
0
5 15 25 35 45 55 65
free T4 (nmol/L)
Figure 4. Correlation of serum hCG vs serum free T4 (r ¼ 0:45; P , 0:001) and serum TSH
(r ¼ 20:48; P , 0:001) in hyperemessis and control subjects. (with permission39). Q 1992 The Endocrine
Society.
Effect of human chorionic gonadotropin on the thyroid 257
140
120
UPTAKE (%)
100
80
125I-IODIDE
60
40
20
0
HYPEREMESIS PREGNANT
GRAVIDARUM CONTROL
200
150
HCG, U/ml
100
50
0
0 50 100 150 200 250 300
IODIDE UPTAKE %
Figure 5. Upper panel, serum thyrotropic activity (measured as iodide uptake in cultured rat cells) in
hyperemeis patients and pregnant controls, mean ^ SE, P , 0:001). Lower panel, correlation of serum hCG
vs serum thyrotropic activity in hyperemesis and pregnant controls, r ¼ 0:50; P , 0:001 (with permission39).
Q 1992 The Endocrine Society.
correlated with the hCG concentration (Figure 5). The authors concluded that hCG
was responsible for the increased hyroid function.
Etiology of hyperemesis gravidarum gravidarum
The etiology of hyperemesis gravidarum gravidarum is unknown. It may be related to the
high hCG level and possibly some action of hCG that is still unclear. The increased thyroid
function, or clinical hyperthyroidism, is attributed to the effect of hCG on the TSH
receptor. The vomiting may be related to increased levels of estradiol, or another steroid
induced by hCG. Although estradiol levels in hyperemesis patients were higher than
those of a control group, there was considerable overlap.39 Increased estradiol levels
were found in women with hyperemesis in the US during the first trimester compared
258 J. M. Hershman
with control subjects.47 A recent study in Greece found that higher levels of estradiol
were associated with nausea with or without vomiting up to the 27th week of
pregnancy.48
Syndrome of transient hyperthyroidsm of hyperemesis gravidarum
The syndrome of transient hyperthyroidsm of hyperemesis gravidarum should be
considered in any woman presenting with biochemical evidence of hyperthyroidism
in early pregnancy. In the vast majority of these patients, there will be spontaneous
remission of the increased thyroid function when the vomiting stops in several
weeks. Antithyroid drug therapy is unnecessary. However, some patients with
hyperemesis have frank clinical hyperthyroidism. Because the clinical hyperthyroid-
ism in these patients differs from that of classical Graves’ disease, it has been called
‘gestational thyrotoxicosis’. It has the following characteristics: thyrotoxic symptoms
in early pregnancy, marked increase in serum FT3 and FT4, association with
hyperemesis gravidarum, spontaneous disappearance in the latter half of pregnancy,
negative thyroid peroxidase antibody, negative TSH receptor antibody, usually an
absence of goiter, and circulating hCG with high biological activity.49
It is be reasonable to treat these patients with antithyroid drugs or a beta-adrenergic
blocker, depending on the clinical features, but treatment is rarely required beyond 22
weeks of gestation. However, there are no controlled clinical trials that can be used for
a guide to management.
Hyperplacentosis, a rare condition in which the placenta is enlarged and hCG
concentration is very high, may cause clinical hyperthyroidism that remits promptly
after delivery of the placenta.50
HCG isoforms with thyrotropic activity
Five patients with gestational thyrotoxicosis and hyperemesis were shown to have
circulating asialo-hCG with high thyrotropic bioactivity.51 Another group confirmed
the potent thyrotropic activity of asialo-hCG in a human thyroid follicle bioassay.52 In
contrast, one study reported a preponderance of acidic variants of hCG in the
serum of patients with hyperemesis gravidarum.35 Another study found a similar
distribution of HCG isoforms in sera of hyperemesis patients and controls36,
however, the thyroid hormone concentrations correlated to the absolute HCG
concentration and the proportion of acidic isoforms. The acidic variants with higher
sialic acid content would be expected to have a longer serum half-life. These reports
support the concept that the absolute amount of HCG plays a role in stimulating
thyroid function.
PLACENTAL TUMORS
Hydatidiform mole
Hyperthyroidism or increased thyroid function has been reported in many patients with
trophoblastic tumors, either hydatiditform mole or choriocarcinoma.33,52 – 54 In the US,
hydatidiform mole occurs between 0.5 and 2.5 per 1000 pregnancies.55 It is more
common in Asian and Latin American countries. The prevalence is greatest in women
Effect of human chorionic gonadotropin on the thyroid 259
over 50 or less than age 15. Women who have had a previous mole have a greater risk
of further molar pregnancies.
The mole consists of vesicles of swollen hydropic villi of various sizes, and there is an
absence of fetal tissue. The karyotype is paternal. The usual clinical presentation is that
of a threatened abortion with vaginal bleeding. In one-half of the patients, the uterus is
large for the date of the pregnancy, About one-fifth of the women have hyperemesis,
and 5 – 10% have toxemia, which is unusual in early pregnancy. The diagnosis is made by
ultrasonography that shows a ‘snowstorm’ appearance without a fetus. The current
widespread use of ultrasound for monitoring pregnancy has resulted in earlier
diagnosis when the tumor mass is smaller.56 In one study, moles were evauated at a
mean gestational age of 8.5 weeks during the period 1994– 97 vs 17.0 weeks during
1969 –75.57 Hydatidiform moles secrete large amounts of HCG, and the HCG level is
proportional to the mass of the tumor.
The prevalence of increased thyroid function in patients with hydatidiform mole has
been reported as 25 –64%.54,55 About 5% have clinical hyperthyroidism.58 In a study of
14 women with hydatidiform mole in 1975, nine were hyperthyroid.53 Serum HCG
levels varied from 150– 3000 U/ml. Thyroid-stimulating activity, measured by bioassay
in mice, was found in all sera, and there was a close correlation between this activity,
the serum HCG, and the T3 level. Removal of the mole caused a dramatic fall in serum
levels of T3, T4, HCG and thytropic activity (Figure 6). The data suggested that HCG,
itself, when present in large amounts that are several-fold the peak levels of pregnancy,
stimulates thyroid function and may cause hyperthyroidism.
32 SERUM T4 800
SERUM T3
T4 µg/100 ml
T3 ng/100 ml
24 600
16 400
8 200
4 100
Nal O.R.
600 1200
HCG
Molar TSH µU/ml
HCG U/ml
Molar TSH
400 800
200 400
0 0
1 2 3 4 5 6 7 8 9 10
DAYS
Figure 6. Serum T4, T3, hCG, and molar TSH (measured by bioassay in mice) in a patient with hydatidiform
mole and hyperthyroidism. She was treated with sodium iodide intravenously and then had evacuation of the
mole by hysterectomy (OR). There was a parallel fall in the hCG and molar TSH concentrations. (with
permission53).
260 J. M. Hershman
The diagnosis of hyperthyroidism, or increased thyroid function, is established by
finding elevated serum free T4 and T3 concentrations and suppressed serum TSH level.
Thyroid radioiodine uptake is greatly increased.59 In general, the development of
hysterotomy requires hCG levels of . 200 U/ml that are sustained for several weeks.
HCG extracted from molar tissue showed molecular heterogeneity with a
significant amount of basic molecules containing less sialic acid than normal, highly
purified HCG.33 The more basic, partially desialylated isoforms of hCG had a much
higher ratio of biologic to immunologic activity than the more acidic forms. The partially
desialylated HCG, because of its greater thyrotropic activity, may be responsible for
hyperthyroidism in some patients with trophoblastic disease. Therefore, the
thyrotropic potency of hCG in patients with trophoblastic disease should be
considered not only based on its immunoreactivity but also on its biological activity.
Therapy consists of evacuation of the mole by suction curettage or removal by
hysterotomy. This results in prompt reduction in thyroid hormone levels, hCG and
thyroid-stimulating activity. Monitoring serum HCG is essential in follow-up to detect
persistence of molar tissue or the development of choriocarcinoma.
Choriocarcinoma
Choriocarcinoma occurs in one in 20 000 to one in 40 000 pregnancies in the US and
Europe.60 About half of the cases occur in women with previously diagnosed
hydatidiform moles, but only 3 –5% of women with moles develop choriocarcinoma.
Patients usually present within 1 year of the previous conception. Pathologically, the
tumors consist of large sheets of syncytiotrophoblastic and cytotrophoblastic cells,
hemorrhage, necrosis and absence of hydropic villi. The tumors invade blood vessels
and progress to hemorrhagic metastases. The natural history is rapid progression,
spread to distant organs, especially lungs and vagina, and less commonly the brain and
liver. Without treatment, death occurs within a few months. Patients present with
vaginal bleeding, hemoptysis if there are lung metastases, focal neurologic signs
indicative of brain metastases, and often profound weight loss.
There have been many case reports of hyperthyroidism in women with
choriocarcinoma.61 – 63 In addition, there are 17 cases of choriocarcinoma in men
usually in testicular tumors, less often in extragonadal sites.64 – 66 The precise
prevalence of hyperthyroidism in patients with trophoblastic tumors is unknown. It
was found in five of 20 patients with trophoblastic disease evaluated at a referral center
in 1 year67, three of these five thyrotoxic patients had choriocarcinoma, and two had
hydatidiform moles. In another study, 30 of 52 patients with gestational trophoblastic
tumors were found to be thyrotoxic.68
Less than 3% of the oligosaccharide side chains of hCG derived from a
choriocarcinoma contained sialic acid, whereas that of normal hCG was mostly
sialylated.69 This is consistent with other reports of the preponderance of basic
isoforms of HCG in trophoblastic tumors.
The principal therapy of choriocarcinoma is chemotherapy. Patients should be
referred to a specialized center. With effective chemotherapy, long-term survival is very
high. In the UK, overall long-term survival exceeds 95%.70 In low-risk disesase the cure
rate is virtually 100%, whereas for high-risk patients it is 86%. Cure of the
choriocarcinoma results in a cure of the hyperthyroidism.61 – 63,67
Effect of human chorionic gonadotropin on the thyroid 261
TSH RECEPTOR MUTATION
A woman with recurrent gestational hyperthyroidism associated with hyperemesis
gravidarum and a TSH receptor mutation was recently reported.71 After two
miscarriages, she had hyperemesis early in pregnancy, along with overt biochemical
hyperthyroidism. She had a small diffuse goiter and no evidence of Graves’ eye
disease. Hyperthyroidism was diagnosed and treated with propylthiouracil through-
out the pregnancy. The drug was discontinued postpartum and normal thyroid
function ensued. During her next pregnancy, she had a recurrence of hyperthyroid-
ism associated with hyperemeis gravidarum, and was again treated with
propylthiouracil.
The patient’s mother had a diagnosis of Graves’ disease during her second and third
gestations. The mother’s first pregnancy was complicated by hyperemesis, and
terminated in miscarriage. During her next pregnancy, she had tremor, tachycardia,
anxiety and hyperemesis. Thyroid function tests revealed hyperthyroidism. She was
treated with antithyroid drugs throughout pregnancy, the hyperemesis resolved, and
she delivered a healthy female baby, the proband. The hyperthyroidism improved in the
postpartum period allowing for discontinuation of antithyroid drugs. The following
80
70
60
Mutant
cAMP Production (pmol/dish)
50
40
30
20 Wild type
10
Mock-transfected cells
0
0 1 33 0 3 10 33 0 0 00
0. 0. 1. 3. 10 30 10
Chorionic Gonadotropin (U/ml)
Figure 7. Functional characteristics of the mutant thyrotropin receptor in COS-7 cells, showing the effect of
stimulation of cAMP production by graded concentrations of hCG in cells transfected with wild-type or
mutant thyrotropin receptor. (with permission71). Q 1998 Massachusetts Medical Society. All rights reserved.
262 J. M. Hershman
pregnancy was also complicated by hyperemesis and hyperthyroidism, requiring
treatment with antithyroid drugs, and followed by recovery of normal thyroid function
postpartum.
Study of the TSH receptor of the patient disclosed the substitution of guanine for
adenine at codon 183 in exon 7 in one allele, resulting in substitution of arginine for
lysine in the middle portion of the extracellular domain of the TSH receptor, a region of
the receptor in contact with the ligand. The patient’s mother was heterozygous for the
same mutation. The mutant TSH receptor was transfected into COS cells and was
shown to be much more sensitive to hCG than the wild-type receptor (Figure 7). It is
likely that the hereditary gestational hyperthyroidism in this family was due to
hypersensitivity of the mutant TSH receptor to hCG. This unique mutation has not yet
been reported in other families.
Recent work has shown that substitution of methionine, asparagjne or glutamine for
the lysine 183 in the TSH receptor increased its affinity toward hCG, the gain of
function was attributed to the release of a nearby glutmate resudue at 157 from a salt
bridge with lysine 183.2
SUMMARY
HCG has thyroid stimulating activity and may cause hyperthyroidism in women with
hyperemesis gravidarum or trophoblastic tumors in women who have high levels of
hCG.
In the vast majority of women with hyperemesis gravidarum, there will be
spontaneous remission of the increased thyroid function when the vomiting stops in
several weeks.
Routine ultrasonography has led to an earlier diagnosis of hydatidiform mole, with a
smaller mass of tumor and lower hCG levels. The development of hyperthyroidism
requires hCG levels of . 200 U/ml that are sustained for several weeks. Removal of the
mole cures the hyperthyroidism. In patients with choriocarcinoma and high hCG levels
causing hyperthyroidsim, the principal therapy is chemotherapy, usually given at a
specialized center.
A unique family with recurrent gestational hyperthyroidism associated with
hyperemesis gravidarum was found to have a mutation in the extracellular domain
of the TSH receptor that made it responsive to normal levels of hCG.
Research agenda
† additional studies should be carried out to characterize the HCG that has
thyroid-stimulating activity in patients with hyperthyroidsm of hyperemesis
gravidarum
ACKNOWLEDGEMENTS
Supported by VA Medical Research Funds.
Effect of human chorionic gonadotropin on the thyroid 263
REFERENCES
1. Pierce JG & Parsons TF. Glycoprotein hormones: structure and function. Annual Review of Biochemistry
1981; 50: 465– 495.
2. Smits G, Govaerts C, Nubourgh I, et al. Lysine 183 and glutamic acid 157 of the TSH receptor: two
interacting residues with a key role in determining specificity toward TSH and human CG. Molecular
Endocrinology 2002; 16: 722–735.
3. Merz WE. Biosynthesis of human chorionic gonadotropin: a review. European Journal of Endocrinology
1996; 135: 269–284.
4. Vassart G & Dumont JE. The thyrotropin receptor and the regulation of thyrocyte function and growth.
Endocrine Reviews 1992; 13: 596– 611.
5. Nagayama Y & Rapoport B. The thyrotropin receptor 25 years after its discovery: new insights after its
molecular cloning. Molecular Endocrinology 1992; 92: 145–156.
6. Kohn LD, Shimura H, Shimura Y, et al. The thyrotropin receptor. Vitamins and Hormones 1995; 50:
287–384.
7. Braunstein GD & Hershman JM. Comparison of serum pituitary thyrotropin and chorionic gonadotropin
concentrations throughout pregnancy. The Journal of Clinical Endocrinology and Metabolism 1976; 42:
1123– 1126.
8. Harada A, Hershman JM, Reed AW, et al. Comparison of thyroid stimulators and thyroid hormone
concentrations in the sera of pregnant women. Journal of Clinical Endocrinology and Metabolism 1979; 48:
793–797.
9. Glinoer D, De Nayer P, Bourdoux P, et al. Regulation of maternal thyroid during pregnancy. Journal of
Clinical Endocrinology and Metabolism 1990; 71: 276–287.
10. Pekonen F, Alfthan H, Stenman UH & Ylikorkala C. Human chorionic gonadotropin (hCG) and thyroid
function in early pregnancy: circadian variation and evidence for intrinsic thyrotropic activity of hCG.
Journal of Clinical Endocrinology and Metabolism 1988; 66: 853 –856.
11. Yoshimura M, Nishikawa M, Ogasawara H, et al. Measurement of erythrocyte Na,K-ATPase activity in
normal pregnant women. Endocrinology Journal 1993; 40: 171– 177.
12. Yoshikawa M, Nishikawa M, Horimoto M, et al. Thyroid-stimulating activity in sera of normal pregnant
women. Journal of Clinical Endocrinology and Metabolism 1989; 69: 891– 895.
13. Kimura M, Amino N, Tamaki H, et al. Physiologic thyroid activation in normal early pregnancy induced by
circulating hCG. Obstetrics Gynecology 1990; 75: 775–778.
14. Hershman JM. Editorial: role of human chorionic gonadotropin as a thyroid stimulator. Journal of Clinical
Endocrinology and Metabolism 1992; 74: 258 –259.
15. Ballabio M, Poshyachinda M & Ekins RP. Pregnancy-induced changes in thyroid function: Role of human
chorionic gonadotropin as putative regulator of maternal thyroid. Journal of Clinical Endocrinology and
Metabolism 1991; 73: 824– 831.
16. Glinoer D. The regulation of thyroid function in pregnancy: pathways of endocrine adaptation from
physiology to pathology. Endocrine Reviews 1997; (“18): 404–433.
17. Yeo CP, Khoo DH, Eng PH, et al. Prevalence of gestational thyrotoxicosis in Asian women evaluated in the
8th to 14th weeks of pregnancy: correlations with total and free beta human chorionic gonadotrophin.
Clinical Endocrinology 2001; 55: 391–398.
18. Nisula BC, Morgan FJ & Canfield RE. Evidence that chorionic gonadotropin has intrinsic thyrotropic
activity. Biochemical and Biophysical Research Communication 1974; 59: 86– 91.
19. Kenimer JG, Hershman JM & Higgins HP. The thyrotropin in hydatidiform moles is human chorionic
gonadotropin. Journal of Clinical Endocrinology and Metabolism 1975; 40: 482–491.
20. Pekary AE, Azukizawa M & Hershman JM. Thyroidal responses to human chorionic gonadotropin in the
chick and rat. Hormone Research 1983; 7: 36–42.
21. Sowers JR, Hershman JM, Carlson HE, et al. Effect of human chorionic gonadotropin on thyroid function
in euthyroid men. Journal of Clinical Endocrinology and Metabolism 1978; 47: 898–901.
22. Hershman JM, Lee HY, Sugawara M, et al. Human chorionic gonadotropin stimulates iodide uptake,
adenylate cyclase, and deoxyribonucleic acid synthesis in cultured rat thyroid cells. Journal of Clinical
Endocrinology and Metabolism 1988; 67: 74 –79.
23. Arturi F, Presta I, Scarpelli D, et al. Stimulation of idide uptake by human chorionic gonadotropin in FRTL-5
cells: effects on sodium/iodide symportere gene and progtein expression. European Journal of Endocrinology
2002; 147: 655–661.
24. Tomer Y, Huber GK & Davies TF. Human chorionic gonadotropin (hCG) interacts directly with
recombinant human TSH receptors. Journal of Clinical Endocrinology and Metabolism 1992; 74: 1477–1479.
25. Yoshimura M, Hershman JM, Pang XP, et al. Activation of the thyrotropin (TSH) receptor by human
chorionic gonadotropin and luteinizing hormone in Chinese hamster ovary cells expressing functional
human TSH receptors. Journal of Clinical Endocrinology and Metabolism 1993; 77: 1009–1013.
264 J. M. Hershman
26. Cole LA & Kardana A. Discordant results in human chorionic gonadotropin assays. Clinical Chemistry 1992;
38: 263–270.
27. Cole LA, Kardana A, Park SY & Braunstein GD. The deactivation of hCG by nicking and dissociation.
Journal of Clinical Endocrinology and Metabolism 1993; 76: 704– 710.
28. Cole LA, Kardana A, Andrade-Gordon P, et al. The heterogeneity of hCG: III. The occurrence, biological
and immunological activities of nicked hCG. Endocrinology 1991; 129: 1559–1567.
29. Yoshimura M, Pekary AE, Pang XP, et al. Effect of peptide nicking in the human chorionic gonadotropin b-
subunit on stimulation of recombinant human thyroid-stimulating hormone receptors. European Journal of
Endocrinology 1994; 130: 92–96.
30. Sairam MR. Role of carbohydrates in glycoprotein hormone signal transduction. FASEB Journal 1989; 3:
1915–1926.
31. Hoermann R, Keutmann HT & Amir SM. Carbohydrate modifications transform human chorionic
gonadotropin into a potent stimulator of adenosine 30 ,50 -monophosphate and growth responses in FRTL-
5 thyroid cells. Endocrinology 1991; 128: 1129– 1135.
32. Pekary AE, Jackson IMD, Goodwin TM, et al. Increased in vitro thyrotropic activity in partially sialated
human chorionic gonadotropin extracted from hydatidiform moles of patients with hyperthyroidism.
Journal of Clinical Endocrinology and Metabolism 1993; 76: 70– 74.
33. Yoshimura M, Pekary AE, Pang XP, et al. Thyrotropic activity of basic isoelectric forms of human chorionic
gonadotropin extracted from hydatidiform mole tissues. Journal of Clinical Endocrinology and Metabolism
1994; 78: 862–864.
34. Hoermann R, Kubota K & Amir SM. Role of subunit sialic acid in hepatic binding, plasma survival rate, and
in vivo thyrotropic activity of human chorionic gonadotropin. Thyroid 1993; 3: 41 –47.
35. Jordan V, Grebe SK, Cooke RR, et al. Acidic isoforms of chorionic gonadotrophin in European and
Samoan women are associated with hyperemesis gravidarum and may be thyrotrophic. Clinical
Endocrinology (Oxford) 1999; 50: 619–627.
36. Talbot JA, Lambert A, Anobile CJ, et al. The nature of human chorionic gonadotrophin glycoforms in
gestational thyrotoxicosis. Clinical Endocrinology (Oxford) 2001; 55: 33–39.
37. Hershman JM. HCG and the thyroid: hyperemesis gravidarum and trophoblastic tumors. Thyroid 1999; 9:
653–657.
38. Al-Yatama M, Diejomaoh M, Nandakumaran M, et al. Hormone profile of Kuwaiti women with
hyperemesis gravidarum. Archives of Gynecology Obstetrics 2002; 266: 218 –222.
39. Goodwin TM, Montoro M, Mestman JH, et al. The role of chorionic gonadotropin in transient
hyperthyroidism of hyperemesis gravidarum. Journal of Clinical Endocrinology and Metabolism 1992; 75:
1333–1337.
40. Bouillon R, Naesens M, Van Assche FA, et al. Thyroid function in patients with hyperemesis gravidarum.
American Journal of Obstetrics and Gynecology 1982; 143: 922 –926.
41. Bober SA, McGill AC & Tunbridge WM. Thyroid function in hyperemesis gravidarum. Acta Endocrinology
1986; 111: 404 –410.
42. Kirshon B, Lee W & Cotton DB. Prompt resolution of hyperthyroidism and hyperemesis gravidarum after
delivery. Obstetrics and Gynecology 1988; 71: 1032–1034.
43. Swaminathan R, Chin RK, Lao TTH, et al. Thyroid function in hyperemesis gravidarum. Acta Endocrinology
1989; 120: 155 –160.
44. Shulman A, Shapiro MS, Behary C, et al. Abnormal thyroid function in hyperemesis gravidarum. Acta
Obstetricia Gynecology Scandinavica 1989; 68: 533–536.
45. Leylek OA, Cetin A, Toyaksi M & Erselcan T. Hyperthyroidism in hyperemesis gravidarum. International
Journal of Gynecology and Obstetrics 1996; 55: 33 –37.
46. Grun JP, Meuris S, De Nayer P & Glinoer D. The thyrotrophic role of human chorionic
gonadotrophin (hCG) in the early stages of twin (versus single) pregnancies. Clinical Endocrinology
1997; 46: 719– 725.
47. Depue RH, Bernstein L, Ross RK, Judd HL & Henderson BE. Hyperemesis gravidarum in relation to
estradiol levels, pregnancy outcome, and other maternal factors: a seroepidemiologic study. American
Journal Obstetrics and Gynecology 1987; 156: 1137–1141.
48. Lagiou P, Tamimi R, Mucci LA, et al. Nausea and vomiting in pregnancy in relation to prolactin, estrogens,
and progesterone: a prospective study. Obstetrics and Gynecology 2003; 101: 639–644.
49. Kimura M, Amino N, Tamaki H, et al. Gestational thyrotoxicosis and hyperemesis gravidarum: possible role
of hCG with higher stimulating activity. Clinical Endocrinology (Oxford) 1993; 38: 345 –350.
50. Ginsberg J, Lewanczuk RZ & Honore LH. Hyperplacentosis: a novel cause of hyperthyroidism. Thyroid
2001; 11: 393–396.
51. Yamazaki K, Sato K, Shizume K, et al. Potent thyrotropic activity of human chorionic gonadotropin
variants in terms of 125I incorporation and de novo synthesized thyroid hormone release in human thyroid
follicles. Journal of Clinical Endocrinology and Metabolism 1995; 80: 473–479.
Effect of human chorionic gonadotropin on the thyroid 265
52. Hershman JM. Hyperthyroidism induced by trophoblastic thyrotropin. Mayo Clinic Proceedings 1972; 47:
913–918.
53. Higgins HP, Hershman JM, Kenimer JG, et al. The thyrotoxic osis of hydatidiform mole. Annals of Internal
Medicine 1975; 83: 307–311.
54. Yoshimura M & Hershman JM. Thyrotropic action of human chorionic gonadotropin. Thyroid 1995; 5:
425–434.
55. Palmer JR. Advances in the epidemiology of gestational trophoblastic disease. The Journal of Reproductive
Medicine 1994; 39: 155–162.
56. Coukos G, Makrigiannakis A, Chung J, et al. Complete hydatidiform mole. A disease with a changing
profile. The Journal of Reproductive Medicine 1999; 44: 698 –704.
57. Mosher R, Goldstein D, Berkowitz R, et al. Complete hydatidiform mole. Comparison of clinocpathologic
features, current and past. The Journal of Reproductive Medicine 1998; 43: 21 –27.
58. Berkowitz RS, Goldstein DP, DuBeshter BE, et al. Management of complete molar pregnancy. The Journal
of Reproductive Medicine 1987; 32: 634–639.
59. Galton VA, Ingbar SH, Jimenez-Fonseca J & Hershman JM:. Alterations in thyroid hormone economy in
patients with hydatidiform mole. The Journal of Clinical Investigation 1971; 50: 1345–1354.
60. Brinton LA, Braken AB & Connelly RR. Choriocarcinoma incidence in the United States. American Journal
Epidemiology 1986; 123: 1094–1100.
61. Cohen JD & Utiger RD. Metastatic choriocarcinoma associated with hyperthyroidism. Journal of Clinical
Endocrinology and Metabolism 1970; 30: 423 –429.
62. Cave Jr. WT & Dunn JT. Choriocarcinoma with hyperthyroidism: probable identity of the thyrotropin with
human chorionic gonadotropin. Annals of Internal Medicine 1976; 85: 60 –63.
63. Morley JE, Jacobson RJ, Melamed J, et al. Choriocarcinoma as a cause of thyrotoxicosis. American Journal of
Medicine 1976; 60: 1036–1040.
64. Karp PJ, Hershman JM, Richmond S, et al. Thyrotoxicosis from molar thyrotropin. Archives of Internal
Medicine 1973; 132: 432 –436.
65. Giralt SA, Dexeus F, Amato R, et al. Hyperthyroidism in men with germ cell tumors and high levels of
beta-human chorionic gonadotropin. Cancer 1992; 69: 1286–1290.
66. Goodarzi MO & Van Herle AJ. Thyrotoxicosis in a male patient associated with excess human chorionic
gonadotropin production by germ cell tumor. Thyroid 2000; 10: 611–619.
67. Rajatanavin R, Chailurkit LO, Srisupandit S, et al. Trophoblastic hyperthyroidism: clinical and biochemical
features of five cases. American Journal of Medicine 1988; 85: 237–241.
68. Desai RK, Norman RJ, Jialal I, et al. Spectrum of thyroid function abnormalities in gestational trophoblastic
neoplasia. Clinical Endocrinology 1988; 29: 583 –592.
69. Mizouchi T, Nishimura R, Derappe C, et al. Structures of the asparagine-linked sugar chains of human
chorionic gonadotropin produced in choriocarcinoma. Journal of Biological Chemistry 1983; 258:
14126–14129.
70. Fisher PM & Hancock BW. Gestational trophoblastic diseases and their treatment. Cancer Treatment
Reviews 1997; 23: 1–16.
71. Rodien P, Bremont C, Sanson ML, et al. Familial gestational hyperthyroidism caused by a mutant
thyrotropin receptor hypersensitive to human chorionic gonadotropin. New England Journal of Medicine
1998; 339: 1823–1826.
You might also like
- Thyrotropic Action of Human Chorionic GonadotropinNo ratings yetThyrotropic Action of Human Chorionic Gonadotropin10 pages
- HCG: Biological Functions and Clinical Applications: Molecular SciencesNo ratings yetHCG: Biological Functions and Clinical Applications: Molecular Sciences15 pages
- hCG in Trophoblastic Disease ManagementNo ratings yethCG in Trophoblastic Disease Management34 pages
- 3.a Link Between High Serum Levels of Human ChorionicNo ratings yet3.a Link Between High Serum Levels of Human Chorionic14 pages
- New Developments in Gonadotrophin Pharmacology: ArticlesNo ratings yetNew Developments in Gonadotrophin Pharmacology: Articles6 pages
- Determination of Hormones: Mohamed A.Ali BSC - HLS, Admls, DmlsNo ratings yetDetermination of Hormones: Mohamed A.Ali BSC - HLS, Admls, Dmls43 pages
- Insert - Elecsys HCG+Beta.07251025500.V7.EnNo ratings yetInsert - Elecsys HCG+Beta.07251025500.V7.En5 pages
- Insert - Elecsys HCG+Beta.09744428500.V1.EnNo ratings yetInsert - Elecsys HCG+Beta.09744428500.V1.En5 pages
- Insert - Elecsys HCG+beta.03271749500.V20.enNo ratings yetInsert - Elecsys HCG+beta.03271749500.V20.en5 pages
- Immunological, Biological: Evidence Gonadotropin Nonpregnant Subjects Has Physical, Chorionic GonadotropinNo ratings yetImmunological, Biological: Evidence Gonadotropin Nonpregnant Subjects Has Physical, Chorionic Gonadotropin5 pages
- Human Chorionic Gonadotropin (HCG) ELISA KIT Cat. No. 0400: ELISA Kits Available From ADI (See Details at The Web Site)No ratings yetHuman Chorionic Gonadotropin (HCG) ELISA KIT Cat. No. 0400: ELISA Kits Available From ADI (See Details at The Web Site)4 pages
- Gestational Trophoblastic Disease: Presented By: DR Tahmeena DR Shweta SR Guide: DR Manjeera Moderator: DR K Usha RaniNo ratings yetGestational Trophoblastic Disease: Presented By: DR Tahmeena DR Shweta SR Guide: DR Manjeera Moderator: DR K Usha Rani78 pages
- Human Chorionic Gonadotropin and Hyperemesis Gravidarum: Experiments of NatureNo ratings yetHuman Chorionic Gonadotropin and Hyperemesis Gravidarum: Experiments of Nature7 pages
- Pregnancy Handbook: "Am I Pregnant?" All B-HCG Levels Explained100% (1)Pregnancy Handbook: "Am I Pregnant?" All B-HCG Levels Explained74 pages
- Implantation and Development Placenta Part 2No ratings yetImplantation and Development Placenta Part 236 pages
- Comportamiento de La Gonadotropina en El Embarazo 240308 192849No ratings yetComportamiento de La Gonadotropina en El Embarazo 240308 19284910 pages
- Purification and Characterization of Human Chorionic GonadotropinNo ratings yetPurification and Characterization of Human Chorionic Gonadotropin10 pages
- Functions P/human - Chorionic - Gonadotropin#FunctionsNo ratings yetFunctions P/human - Chorionic - Gonadotropin#Functions2 pages
- Thyroid Hormones in Human Follicular Fluid and Thyroid Hormone Receptor in Human Granulosa CellsNo ratings yetThyroid Hormones in Human Follicular Fluid and Thyroid Hormone Receptor in Human Granulosa Cells4 pages
- Human Chorionic Gonadotropin HCG 2nd Edition Digital Test BankNo ratings yetHuman Chorionic Gonadotropin HCG 2nd Edition Digital Test Bank303 pages
- Genetic Variability in Romosinuano-Zebu CattleNo ratings yetGenetic Variability in Romosinuano-Zebu Cattle11 pages
- Understanding Functions and Their Representations100% (1)Understanding Functions and Their Representations20 pages
- Attorney-General and Another V WhitemanNo ratings yetAttorney-General and Another V Whiteman10 pages
- Jayant Vishnu Narlikar - The Great Astrophysicist Believed It's Essential To Have Voices Who Question Mainstream DogmaNo ratings yetJayant Vishnu Narlikar - The Great Astrophysicist Believed It's Essential To Have Voices Who Question Mainstream Dogma1 page
- Primary Health Care Expectations and Reality of Bangladesh1No ratings yetPrimary Health Care Expectations and Reality of Bangladesh117 pages
- Strategic Importance of Human Resource ManagementNo ratings yetStrategic Importance of Human Resource Management21 pages
- Second Term exam-WPS Office Home Economics J 1 & 2No ratings yetSecond Term exam-WPS Office Home Economics J 1 & 25 pages
- Boolean Algebras, Boolean Rings and Stone's Representation TheoremNo ratings yetBoolean Algebras, Boolean Rings and Stone's Representation Theorem8 pages
- Hidden Meaning of Kurma Avtaar ExplainedNo ratings yetHidden Meaning of Kurma Avtaar Explained212 pages
- IELTS Speaking Assessing Lexical ResourceNo ratings yetIELTS Speaking Assessing Lexical Resource10 pages
- Marketing Management 2 - Final Exam: QuestionsNo ratings yetMarketing Management 2 - Final Exam: Questions1 page