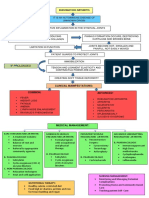
TREATMENT AND MANAGEMENT OF RHEUMATOID
ARTHRITIS
The treatment and management of rheumatoid arthritis (RA) focus on reducing symptoms, like
controlling inflammation, preventing joint and organ damage, and improving quality of life.
Here’s the treatment options available for rheumatoid arthritis:
1. MEDICATIONS:
RA treatment often requires a combination of drugs tailored to the
individual. Common categories include:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These help in relieving pain and
reduce inflammation.
E.g. ibuprofen and naproxen. Ibuprofen: 400-800 mg orally every 6-8 hours as needed
Naproxen: 250-500 mg orally twice daily.
Corticosteroids:These drugs can reduce inflammation and slow joint damage. However,
they are usually used short-term due to potential side effects.
E.g. Prednisone: Typically 5-10 mg daily for maintenance but can go up to 20 mg for short-
term use in flare-ups.
Disease-Modifying Antirheumatic Drugs (DMARDs): These are the cornerstone of RA
treatment, targeting the immune system to slow disease progression. E.g. Methotrexate is
a common first-line DMARD.
E.g. Methotrexate: 7.5-25 mg once weekly, often taken with folic acid (1 mg daily) to reduce
side effects.
Biologic Response Modifiers (Biologics): These are a type of DMARD targeting
specific parts of the immune system. Examples include TNF inhibitors (such as
adalimumab and infliximab) and interleukin inhibitors. They are often prescribed for
patients who don’t respond to traditional DMARDs.
E.g. Adalimumab: 40 mg subcutaneously every other week.
Etanercept: 50 mg subcutaneously once weekly.
Janus Kinase (JAK) Inhibitors: These are newer medications that can be taken orally.
They work by blocking specific enzymes involved in the immune response.
E.g. Tofacitinib: 5 mg orally twice daily or 11 mg once daily
Supplements: Omega-3 fatty acids (fish oil) and turmeric (curcumin) are popular
supplements for reducing inflammation. Always consult with a doctor before adding
supplements.
2. PHYSICAL THERAPY AND EXERCISE:
Physical Therapy: A physical therapist can help design an exercise program to improve
flexibility, strength, and endurance, which supports joint health and function.
Regular Exercise: Low-impact aerobic exercises, such as swimming, walking, and
cycling, are generally recommended. Strengthening and stretching exercises help
improve joint stability and flexibility.
Occupational Therapy: An occupational therapist can provide adaptive devices such as
Assistive Devices like Braces, splints, and other devices help reduce strain on affected
joints.
3. LIFESTYLE MODIFICATIONS:
Weight Management: Maintaining a healthy weight helps reduce stress on the joints,
particularly in the knees and hips, and can improve RA symptoms.
Healthy Diet: An anti-inflammatory diet rich in fruits, vegetables, lean proteins, and
omega-3 fatty acids (found in fish oil) may help reduce inflammation.
Quit Smoking: Smoking is a known risk factor for developing RA, and quitting can
improve symptoms and response to treatment.
4. SURGICAL OPTIONS:
Surgery may be considered if RA leads to severe joint damage
that limits mobility or causes intense pain. Options include:
Synovectomy: Removal of the inflamed synovium (joint lining).
Joint Fusion (Arthrodesis): Fusion of bones to stabilize and reduce pain in a joint.
Total Joint Replacement(Arthroplasty): Replacing the damaged joint with an artificial
one, most commonly in the knees and hips.
REFERENCE:
https://my.clevelandclinic.org/health/diseases/4924-rheumatoid-arthritis
Gaffo, A., Saag, K. G., & Curtis, J. R. (2006). Treatment of rheumatoid arthritis.
American journal of health-system pharmacy, 63(24), 2451-2465.