Traumatic spinal cord injury isn’t just a one-time event but also a chronic condition. Furthermore, people with a history of spinal cord injury are more likely to develop cardiovascular, neurological, psychiatric, and endocrine diseases—regardless of age, location of injury, or prior health status.
These are two key takeaways from research led by Mass General Brigham investigators published in JAMA Network Open.
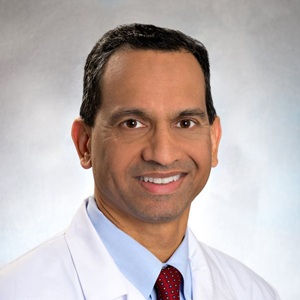
“We have shown not only that these multisystem comorbidities are happening after spinal cord injury but also that they are associated with increased mortality risk,” says the corresponding author, neurologist Saef Izzy, MD, MBChB, FNCS, FAAN. “It’s time for action. We urgently need more programs that focus on screening and prevention in these patients.”
Building on Previous Research on Traumatic Brain Injury
Dr. Izzy, principal investigator of the Izzy Lab at Brigham and Women’s Hospital and head of the Brigham’s Immunology of CNS Injury Program, has led several studies analyzing the downstream effects of traumatic brain injury.
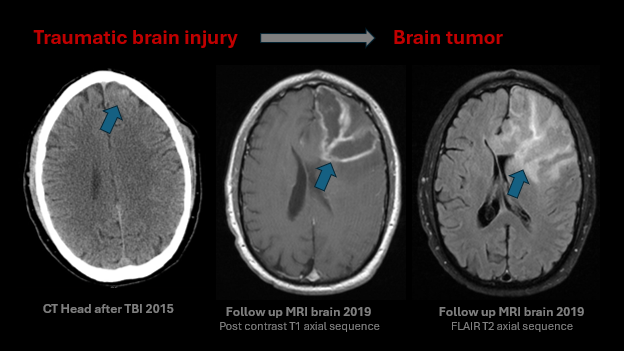
Another 2025 paper published in JAMA Network Open suggested that traumatic brain injury is a chronic condition that raises the risk of developing a malignant brain tumor. Earlier papers documented other long-term clinical consequences of brain injury, including heightened risks of cardiovascular, psychiatric, and other diseases.
Given the results of these and other studies, the researchers note in the new paper, “It is…possible that (traumatic spinal cord injury) can similarly increase the risk of systemic diseases.” The study is the first large cohort analysis to frame spinal cord injury as a chronic disease.
Dr. Izzy and his colleagues tracked the health of 1,038 patients with traumatic spinal cord injury treated at Mass General Brigham and 1,711 patients with spinal cord injury treated at the University of California Health System between January 1996 and January 2024. Over a follow-up period of up to 20 years, the researchers documented the incidence of chronic conditions and death in the patient group. These data were used to compare outcomes with matched control subjects without spinal cord injury.
Compared to the healthy control group, patients with a history of traumatic spinal cord injury had a significantly higher long-term risk of:
- Cardiovascular conditions such as hypertension, hyperlipidemia, ischemic stroke, coronary artery disease, and diabetes
- Neurological conditions such as dementia and seizures
- Psychiatric conditions such as depression
- Endocrine conditions such as erectile dysfunction and adrenal insufficiency
“Interestingly, the risk of these comorbidities was independent of prior brain injury,” Dr. Izzy says.
The researchers also found that traumatic spinal cord injury was associated with an increased risk of death, even in previously healthy patients.
A Call for Long-term, Multidisciplinary Care Strategies
Dr. Izzy says the study findings point to the need for long-term, multidisciplinary care strategies for managing individuals with spinal cord injury, including:
- Implementing routine screening to identify patients at higher risk for an array of comorbidities
- Educating primary care physicians on asking about spinal cord injury history when evaluating conditions like hypertension, as patients may have more extensive follow-up needs
- Establishing a structured follow-up schedule for patients after discharge from the hospital, rehabilitation, or nursing home
- Setting up EMR-based flags or care bundles to automatically identify patients with spinal cord injury history and prompt clinicians to schedule appropriate surveillance
- Prioritizing early detection and timely intervention to optimize outcomes, including reducing mortality risk
The study authors acknowledge several limitations in the paper. Most prominently, the study relied on ICD codes that physicians entered to identify patient conditions. Although there is a strong correlation between codes and new diagnoses, patients with pre-existing conditions were excluded. Therefore, the results may be more applicable to individuals who were healthier at the beginning of the study period and may underestimate the incidence of chronic conditions among traumatic spinal cord injury patients.
“While this isn’t a prospective cohort yet, it provides an important foundation,” Dr. Izzy says. “Our goal is to build on these findings with a long-term prospective study following patients for 10 years or more. With support from research foundations and the National Institutes of Health, we can launch that next phase and generate even more definitive evidence.”
For now, Dr. Izzy and his colleagues at Mass General Brigham are focused on building collaborations with other institutions in the hopes of conducting more extensive studies of spinal cord injury patients at high risk of specific comorbidities.
“Expanding the number of patients will enable more refined endophenotyping of these cohorts,” Dr. Izzy says. “This will help us better understand how to monitor individuals over time and develop strategies to reduce long-term chronic disease burden.”
His recent work on traumatic spinal cord injury and traumatic brain injury is reshaping how clinicians—including Dr. Izzy himself—understand and approach these conditions.
“Ten years ago, we suspected these connections, but we didn’t yet have the data to prove them,” Dr. Izzy says. “Today, the evidence shows a strong epidemiologic link between brain and spinal trauma and a broad spectrum of chronic diseases. The next step is clear: earlier screening, smarter prevention, and better long-term care for patients.”